Is It Easy to Fracture Your Thumb
Bennett Fracture is an articular fracture of the base of the thumb metacarpal consisting of a single, variable-sized, volar-ulnar fracture fragment.
Mechanism of injury
Bennett fracture is really a fracture subluxation. The injury occurs when the thumb metacarpal is axially loaded and partially flexed.
The Bennett fragment is of variable size, is pyramidal in shape, and consists of the volar-ulnar aspect of the metacarpal base.
The anterior oblique ligament, which runs from the fractured fragment to the trapezium, holds the fragment in anatomic position.
See Also: Hand Anatomy
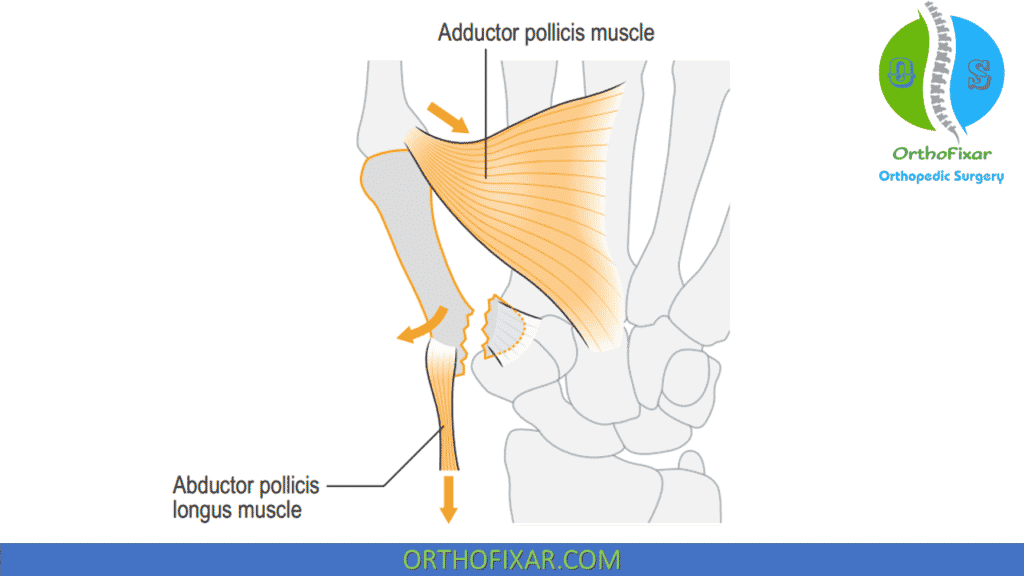
Deforming Forces
A small volar lip fragment of the metacarpal base remains in an anatomical and stable position attached to the trapezium. The remainder of the metacarpal and the thumb, however, are displaced proximally and into adduction and supination.
- Abductor pollicis longus (APL) and thumb extensors cause proximal, dorsal, and radial displacement of the metacarpal shaft.
- Adductor pollicis causes supination and adduction of the metacarpal shaft.
- Anterior oblique or "beak" ligament keeps the volar-ulnar base fragment reduced to trapezium.
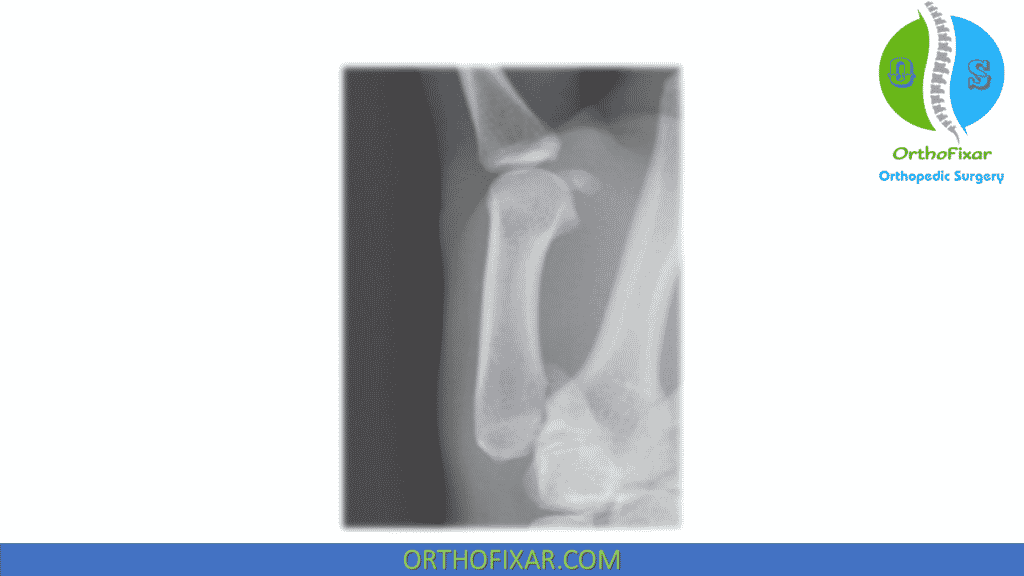
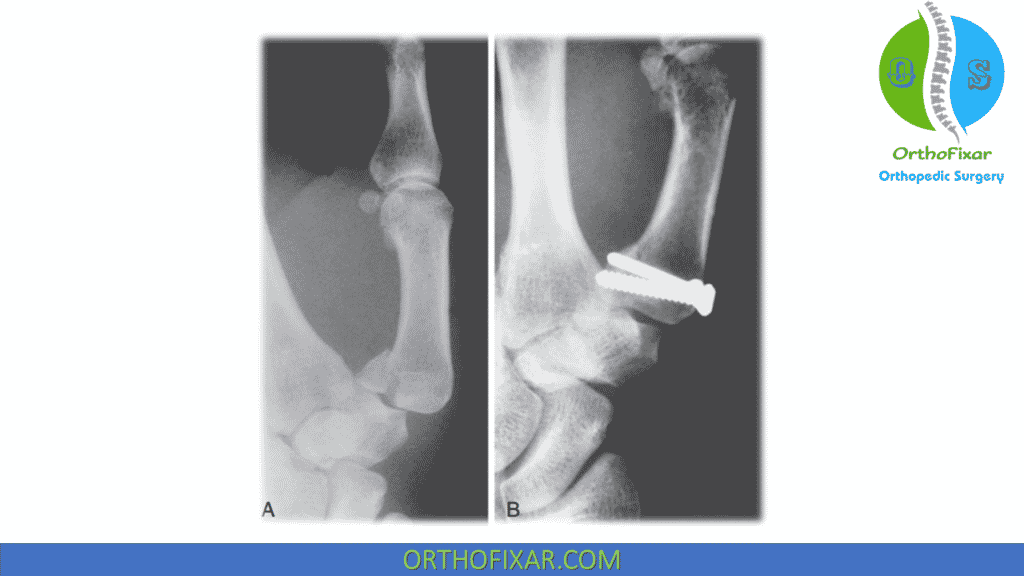
Radilology
X-ray imaging is good to diagnosis the fracture, best seen on hyper-pronated thumb view.
Bennett Fracture Treatment
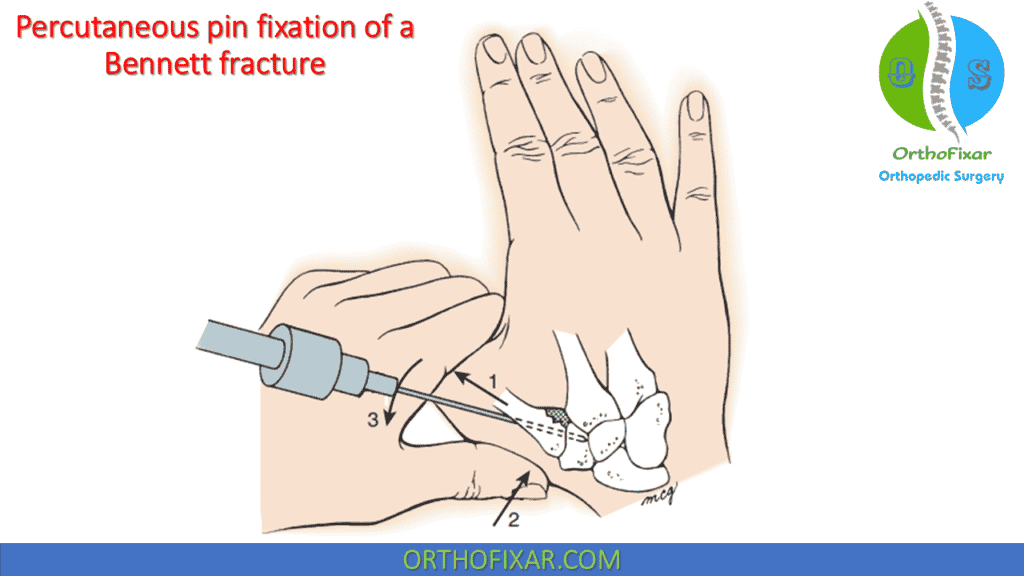
Bennett Fracture Reduction Maneuver
When the Bennett's fracture fragment is less than 15% to 20% of the articular surface, closed reduction and percutaneous pinning of the CMC joint is recommended:
- Under regional or general anesthesia, the thumb metacarpal is extended and pronated, while longitudinal traction and downward pressure are applied to the metacarpal bas.
- While the reduction is held, a Kirschner wire is drilled obliquely across the trapeziometacarpal joint under fluoroscopic guidance.
- The reduction, articular congruity, and pin position are checked with the image intensifier.
- If the metacarpal is reduced to the Bennett fragment and there is less than 2 mm of articular step-off, we accept the reduction and immobilize the digit in a thumb spica cast.
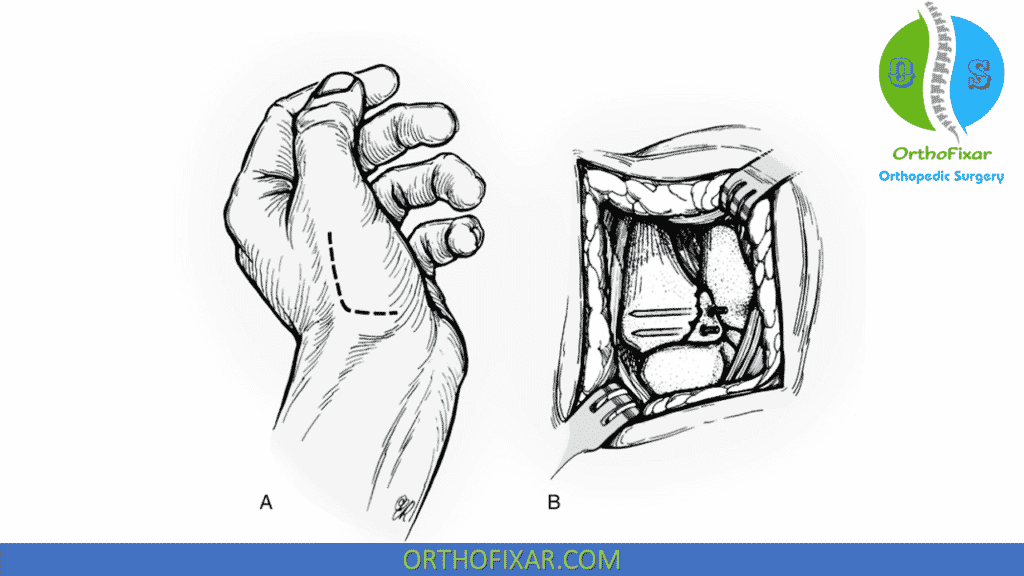
If the Bennett fragment is irreducible, ORIF is recommended:
- The joint is approached through a Wagner incision. The longitudinal limb of this incision is over the subcutaneous border of the thumb metacarpal (between the abductor pollicis longus and the thenar muscles) and is extended proximally and ulnarly to the radial border of the flexor carpi radialis.
- The thenar muscles are reflected subperiosteally, the joint capsule is incised, and the fracture is visualized. When articular congruity has been restored, the articular fragment is held reduced with either reduction forceps or a small bone hook. Fixation of large fragments is secured with either a 1.5-mm or 2-mm lag screw, as suggested by Foster and Hastings.
- For smaller fragments, 0.035-inch Kirschner wires can be placed across the fracture.
- With pin fixation, it is advisable to protect the reduction with an additional transarticular pin.
Postoperatively, if pins are used, the thumb is immobilized in a thumb spica cast for 4 weeks, and the transarticular pin is removed. The pins holding the fracture fragment are removed at 6 weeks. Screw fixation, although technically more demanding, is more secure, and active range of motion may be initiated 5 to 10 days postoperatively.
Treatment Studies
Before the 1970s, nonoperative Bennett Fracture treatment was the rule, and controversy regarding the need for anatomic reduction persists today. Most authors recommend an attempt at improvement of the metacarpal subluxation with percutaneous or open reduction. Cannon and coworkers evaluated patients nearly 10 years after nonoperative management and noted little evidence of symptomatic arthritis despite imperfect reduction. Kjaer-Petersen and colleagues noted a higher incidence of symptomatic arthritis when articular incongruity persisted after reduction. Livesley observed 17 patients for 26 years after closed reduction and casting. All patients had diminished mobility and strength, and most had radiographic evidence of degenerative arthritis and joint subluxation. Livesley concluded that this fracture should not be managed conservatively.
Numerous techniques for closed reduction and percutaneous fixation have been recommended. Closed reduction and fluoroscopically guided percutaneous pinning from the thumb metacarpal into the trapezium without anatomic restoration of the metacarpal articular surface has become increasingly popular. Another technique is Kirschner pin fixation between the first and second metacarpals (intermetacarpal pinning) as advocated by van Niekerk and Ouwens.
Timmenga and associates bserved patients nearly 11 years after percutaneous or open reduction of a Bennett fracture. They concluded that exact reduction should be the aim of treatment. Most of their patients had some degenerative changes radiographically, but there was no correlation with symptoms.
Lutz and associates assessed the long-term functional outcome of 32 patients with Bennett fractures with an articular step-off of less than 1 mm. They noted no difference in clinical outcome or incidence of osteoarthritis between percutaneous and open reduction in treatment of Bennett fractures. They recommended percutaneous reduction for fracture-dislocations with a large beak fragment and open reduction for irreducible fractures. If the Bennett fragment is of adequate size, internal fixation with a screw can be performed.
Complications
- Long-standing instability with painful arthritis is best treated by a trapeziometacarpal joint arthrodesis.
- Nonunion is practically unknown.
- A contracture of the first web can result if the thumb metacarpal has been immobilized in an adducted position.
References
- Cannon SR, Dowd GS, Williams DH, Scott JM. A long-term study following Bennett's fracture. J Hand Surg Br. 1986 Oct;11(3):426-31. doi: 10.1016/0266-7681(86)90172-5. PMID: 3794490.
- Kjaer-Petersen K, Langhoff O, Andersen K: Bennett's fracture. J Hand Surg [Br] 15:58–61, 1990.
- Livesley PJ: The conservative management of Bennett's fracture-dislocation: a 26-year follow-up. J Hand Surg [Br] 15:291–294, 1990
- Lutz M, Sailer R, Zimmermann R, et al: Closed reduction transarticular Kirschner wire fixation versus open reduction internal fixation in the treatment of Bennett's fracture dislocation. J Hand Surg [Br] 28:142–147, 2003.
- van Niekerk JL, Ouwens R: Fractures of the base of the first metacarpal bone: results of surgical treatment. Injury 20:359–362, 1989
- Timmenga EJ, Blokhuis TJ, Maas M, et al: Long-term evaluation of Bennett's fracture: a comparison between open and closed reduction. J Hand Surg [Br] 19:373–377, 1994
- Wagner CJ: Method of treatment of Bennett's fracture dislocation. Am J Surg 80:230–231, 1950
- Foster RJ, Hastings H, 2nd: Treatment of Bennett, Rolando, and vertical intraarticular trapezial fractures. Clin Orthop Relat Res 214:121–129, 1987.
- Greens Operative Hand Surgery 7th Edition Book.
Source: https://orthofixar.com/trauma/bennett-fracture-thumb/
Belum ada Komentar untuk "Is It Easy to Fracture Your Thumb"
Posting Komentar